When Community Holds the Mirror
Last night I attended a Cease Fire meeting in South Los Angeles. It was a room filled with community leaders, service providers, outreach workers, and people who live with the consequences of the systems we build. Many of them work directly with people experiencing homelessness. Some of them discharge to Soul Housing. Some of them have referred to our Recuperative Care program for years. A few of them have been harmed by failures in the past.
It was a necessary room to sit in.
Work like ours often happens behind gates, inside programs, inside policies, inside well-intentioned frameworks. Over time it becomes easy to measure success by internal metrics and operational improvements. What is harder, and more important, is staying close to the lived experience of the people who are impacted when things go wrong.
I met a former participant who was discharged during a difficult transition period. At the time, communication failed and transitions were not handled with the care they should have been. He ended up back on the street. He survived through his own resilience, but with unnecessary hardship layered on top of an already fragile situation. That hardship did not need to happen.
There were also hard questions about broken promises made long before our current leadership and structure existed. Promises that were remembered clearly by the people they were made to. Promises that shaped trust, and when broken, shaped anger. That anger was justified.
This is the part of the work that does not show up in reports or dashboards. It shows up in rooms like that one. It shows up years later. It shows up in the faces of people who remember what it felt like to be dismissed, rushed, or treated as an operational problem instead of a human being.
What mattered just as much, though, was what came alongside the accountability.
There was recognition that we have changed. That we have slowed down in the right places. That we are more structured, more transparent, and more intentional about how people move through care. Community partners who recently walked our facilities spoke about professionalism, compassion, and improvement. That feedback matters, not as validation, but as confirmation that change is visible beyond our own walls.
Progress in this space is rarely clean or linear. It requires correcting course while still moving forward. It requires acknowledging harm without letting past failures define the future. It requires listening more than explaining, and showing up even when it is uncomfortable.
The takeaway from that meeting was not that the work is failing. It was that the work demands constant engagement with the community it serves. Not only when things are going well, and not only through intermediaries, but face to face, consistently, and with humility.
If we want to do this work well, we cannot operate in isolation. We have to look beyond our own programs and metrics and remember that trust is built in moments, and lost the same way. Being better is not about being perfect. It is about being accountable, responsive, and willing to learn in public.
That is the standard worth holding ourselves to.
America is at an inflection point in homeless healthcare
An in-depth, nonpartisan analysis of homeless healthcare at a national inflection point. Examines 1115 and 1915(b) Medicaid waivers, Coordinated Entry Systems, and the need for stabilization before housing. Highlights recuperative care and long-term program stability using Soul Housing Recuperative Care as an example.
Over the past decade, homelessness policy has increasingly centered on housing as the primary solution. Housing remains essential and should always be the long-term goal. But as homelessness becomes more medically complex, behaviorally acute, and systemically entrenched, it is becoming clear that housing alone cannot carry the full weight of the response.
What is emerging now is not a left-right debate, but a systems problem.
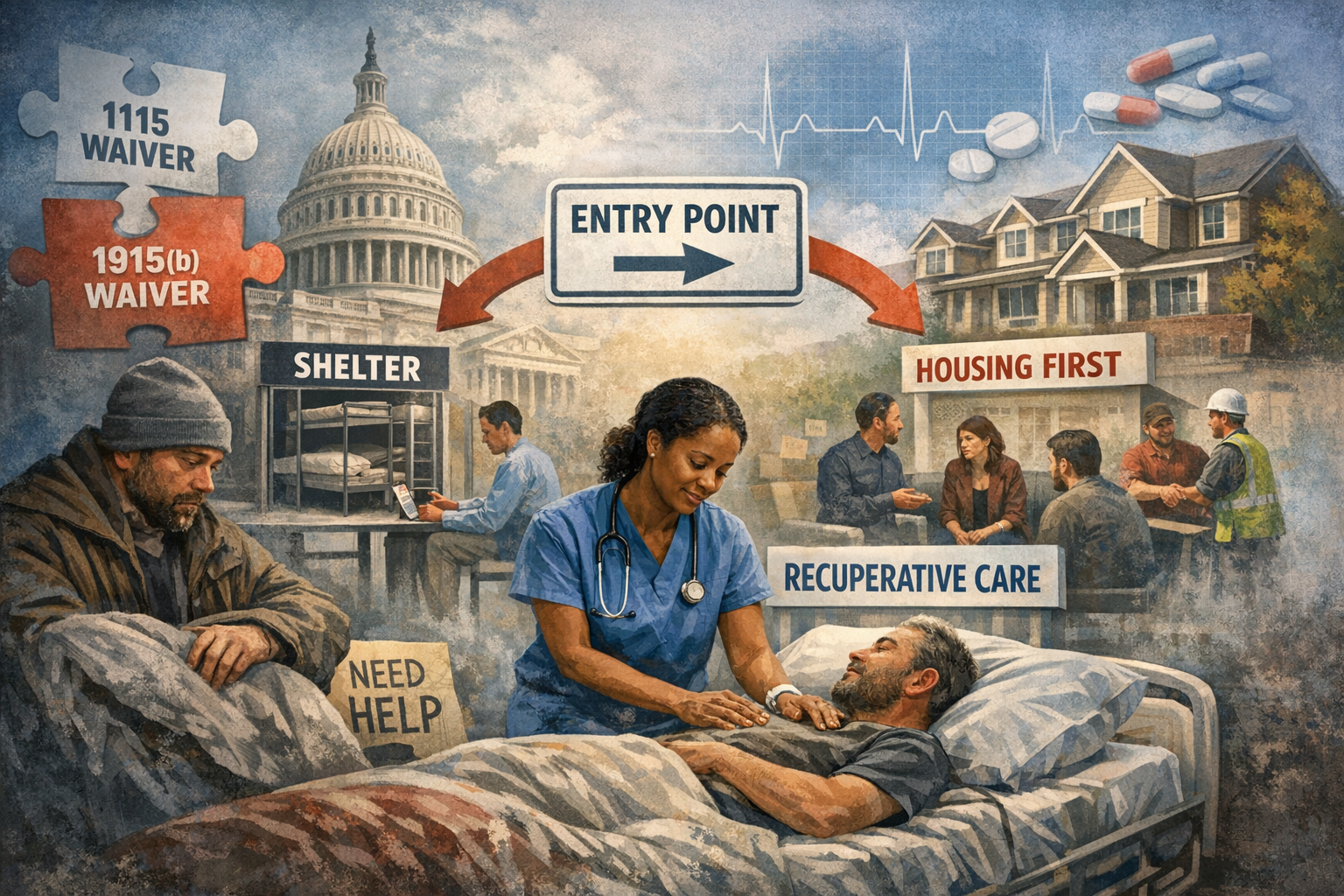
Across the country, communities are relying heavily on federal Medicaid waiver authority, particularly Section 1115 demonstration waivers and Section 1915(b) managed care waivers, to fund healthcare services tied to homelessness. These waivers have enabled critical innovations, including recuperative care, medical respite, enhanced care management, and housing-related supports. At the same time, they introduce uncertainty into a moment that demands stability.
Waivers, by design, are temporary. They are subject to renewal cycles, shifting federal guidance, state interpretation, and political change. Programs built on waiver authority often operate on short planning horizons, even as the populations they serve require long-term, consistent intervention. This mismatch is increasingly visible on the ground.
Healthcare providers, counties, and managed care plans are being asked to scale programs for people with complex medical, mental health, and substance use needs while funding structures remain provisional. The result is fragmentation. Services expand, retract, rebrand, and reconfigure, often faster than frontline systems can absorb.
This instability shows up most clearly at the point of entry.
In many counties, the Coordinated Entry System, or CES, functions primarily as a housing prioritization tool. It was designed to allocate scarce housing resources fairly, not to serve as a clinical or stabilization gate. Over time, however, CES has become the de facto front door for people with needs that extend well beyond housing.
This creates a structural gap.
Housing is the destination, but stabilization is the prerequisite. Many individuals experiencing homelessness are not immediately housing-ready, even when units are available. Untreated medical conditions, unmanaged mental illness, active substance use, and lack of basic daily functioning can make rapid placement unsuccessful or unsustainable. When stabilization is skipped, housing placements fail, costs rise, and individuals cycle back into crisis.
This is not an argument against housing-first principles. It is an argument for sequencing.
Stabilization does not mean delay or denial. It means meeting people where they are clinically and functionally, addressing acute needs first, and creating a realistic pathway to housing that can endure. Medical respite and recuperative care programs are designed precisely for this role, providing a short-term, structured environment where individuals can recover, stabilize, and reconnect to care before moving forward.
At organizations like Soul Housing Recuperative Care, this model is applied daily. Participants are referred not because they need housing, but because they need time and support to recover from illness or injury in a safe setting. During that window, medical care is coordinated, behavioral health needs are identified, substance use treatment options are engaged when appropriate, and basic routines are reestablished. Housing planning happens in parallel, not in isolation.
This approach highlights a broader lesson. Homelessness is not a single condition. It is the outcome of overlapping systems failures, including healthcare access, behavioral health capacity, workforce participation, and social support. Treating it as a housing logistics problem alone oversimplifies reality and limits outcomes.
The current reliance on 1115 and 1915(b) waivers reflects innovation, but also fragility. When core stabilization services depend on temporary authority, the entire continuum becomes vulnerable to disruption. Providers hesitate to invest, counties struggle to plan, and individuals experience inconsistent access to care.
What is needed now is not ideological realignment, but structural clarity.
Stable programs require stable authorization. Clear clinical gates must complement housing prioritization. Healthcare, behavioral health, and recovery services must be treated as foundational infrastructure, not auxiliary supports. And data must be used to evaluate not just placement speed, but durability of outcomes.
The next phase of homeless healthcare will be defined by whether systems can move from pilots to permanence. Housing will remain the goal. But without deliberate investment in stabilization, the system will continue to recycle people through crisis rather than resolve it.
This is the inflection point. The decisions made now about structure, sequencing, and permanence will shape outcomes for years to come.
Fraud, Guardrails, and Accountability in Medicaid-Funded Community Support Services
ederal scrutiny of Medicaid-funded community support services is increasing nationwide. The issue is not whether recuperative care should exist, but how it is structured. Clear guardrails, defined medical necessity, and operational discipline are essential to reducing fraud while preserving access to care.
Federal enforcement activity around Medicaid-funded community support services has increased nationwide. Oversight agencies are focusing on billing integrity, medical necessity, referral practices, and program structure across services that operate at the intersection of healthcare delivery and homelessness response. This includes recuperative care, medical respite, housing navigation, and post-discharge stabilization programs.
This scrutiny is not ideological. It reflects a system that expanded rapidly through waivers, pilots, and emergency authorities without consistent national standards. As these services mature, enforcement actions are increasingly aimed at correcting structural weaknesses that allow misuse of public funds rather than eliminating the services themselves.
Recuperative care exists to address a defined medical gap. It serves individuals who are stable enough to be discharged from a hospital but not stable enough to recover on the street or in a traditional shelter. When properly designed, recuperative care reduces avoidable inpatient days, lowers emergency department utilization, and improves continuity of care. When improperly structured, it becomes vulnerable to fraud risk, overbilling, or misclassification as housing.
Most federal fraud findings in this space stem from predictable failure points. These include billing without documented medical necessity, extending lengths of stay beyond authorized limits, duplicative billing across programs, retroactive referrals, and unclear separation between healthcare services and room and board. These risks are structural, not political, and they appear across states, providers, and administrations.
Guardrails are the primary mechanism for fraud reduction.
Clear program definitions are foundational. Recuperative care must remain time-limited and medically indicated, with objective admission and discharge criteria. Lengths of stay should be capped and enforced. Re-entry rules must be explicit. Programs that drift into open-ended housing models or operate without exit accountability increase both financial exposure and enforcement risk.
Documentation discipline is equally critical. Every billed day must align with a clinical rationale, recovery activity, or care coordination function. This does not require excessive paperwork, but it does require consistency. Intake assessments, daily service logs, discharge planning, and transition outcomes must align in both timing and substance. Delayed or retroactive documentation remains one of the most common audit triggers nationwide.
Operational separation also plays a central role in compliance. Healthcare recovery services, housing navigation, and shelter operations should be clearly delineated, even when delivered by affiliated entities. This separation reduces conflicts of interest and ensures billing accuracy. Programs that control intake, placement, length of stay, and billing without independent checks face heightened scrutiny.
Technology can support accountability when applied correctly. Real-time census tracking, standardized intake workflows, auditable logs, and presence verification systems help confirm that services billed were actually delivered. These tools function as compliance safeguards, not surveillance mechanisms, and protect patients, providers, and payers alike.
At companies like Soul Housing Recuperative Care, Evergreen Medical Respite Care, and North Star Recuperative Care, operational design has focused on maintaining these guardrails as programs scale. Clear service boundaries, capped lengths of stay, disciplined documentation, and defined transition pathways are treated as compliance requirements rather than administrative burdens. This reflects a broader shift within the field toward defensible, repeatable models that can withstand audit and enforcement scrutiny.
Federal enforcement trends should not be interpreted as opposition to community-based care. They signal maturation. Services that originated under temporary authorities must evolve into standardized, accountable systems if they are to remain viable long-term.
Well-designed guardrails benefit all stakeholders. Patients receive care that is appropriate and timely. Hospitals gain reliable discharge partners. States and managed care plans reduce financial leakage. Ethical providers are no longer undercut by programs willing to operate without structure.
Recuperative care and related community support services are likely to remain core components of the healthcare continuum. Their sustainability will depend not on rhetoric, but on design. Clear rules, enforced limits, transparent documentation, and operational discipline are the foundation for reducing fraud while preserving access to medically necessary care.
Legitimacy in this space is built through structure.
America’s Older Homeless Crisis Is a Healthcare Failure.
Older Americans are becoming homeless due to a federal healthcare gap between Medicare discharge and recovery. Why recuperative care must become permanent Medicaid policy.
Older Americans are becoming homeless at a faster rate than any other age group in the country. Adults over 55 now represent roughly one in five people experiencing homelessness nationwide, and the numbers continue to rise. This trend is often framed as a housing affordability issue or a social services failure. In reality, it is the predictable result of a structural gap in federal healthcare policy.
For many older adults, homelessness begins with a medical event. A hospitalization. A fall. A surgery. A behavioral health crisis. Medicare pays for the acute care. The patient stabilizes. And then the system runs out of options.
When an older adult no longer meets inpatient criteria and does not qualify for a skilled nursing facility or inpatient rehabilitation, Medicare coverage effectively ends. The patient is medically cleared, even if they have nowhere safe to recover. Shelters are inappropriate. Housing placement is not immediate. Returning to the street or an unsafe environment leads to rapid decline, emergency department visits, and readmission.
This is not an individual failure. It is a discharge failure.
The Missing Link Between Medicare Discharge and Recovery
Medicare is designed to pay for defined medical services. It is not designed to cover short-term medical stabilization outside institutional settings. There is no Medicare benefit for recuperative care or medical respite. There is no coverage for time-limited, non-skilled step-down care when a patient is too fragile for shelter but no longer qualifies for inpatient services.
That gap has consequences.
Hospitals hold patients longer than medically necessary because there is nowhere safe to send them. Emergency departments back up. Older adults are discharged anyway when beds are needed, often into conditions that guarantee deterioration. The costs return to Medicare through avoidable readmissions and emergency care. The human cost is measured in shortened lives.
Why Medicaid Is the Only Tool That Can Close the Gap
Many older adults experiencing homelessness are dually eligible for Medicare and Medicaid, or they become Medicaid-eligible following a destabilizing health event due to poverty, disability, or spend-down. For this population, Medicaid becomes the only payer capable of covering services Medicare excludes.
That is why recuperative care exists today under Medicaid authority rather than Medicare. Not because it is housing. Because it fills a medical stabilization gap Medicare was never built to address.
States currently rely on temporary Medicaid waivers and demonstrations to fund recuperative care. These programs work, but they are unstable. States must repeatedly reapply for authority. Rules vary widely. Capacity is limited. Oversight is inconsistent. Providers cannot plan long term. Patients lose access when pilots expire.
This is not a problem of evidence. It is a problem of federal policy design.
Recuperative Care Is Healthcare Infrastructure, Not a Housing Program
Recuperative care is a short-term medical stabilization setting for individuals who are clinically appropriate to leave acute care but not appropriate for shelter, housing placement, or return to the originating setting without support. It focuses on physical recovery, behavioral health stabilization, medication adherence, and continuity of care. It is time-limited. It is medically indicated. It is not housing and it is not open-ended.
Well-run recuperative care programs operate with hard guardrails:
Length of stay capped, typically at 90 days
Admission and continued stay determined by licensed clinicians
Mandatory transition planning beginning at admission
No authority over housing placement or custody decisions
Utilization review and outcome-focused audits
These programs reduce avoidable inpatient days, lower readmissions, and create a predictable bridge between acute care and whatever comes next. They are already doing this in states across the country.
Soul Housing has spent years operating within these constraints, stabilizing medically vulnerable individuals who would otherwise cycle between hospitals and the streets. The work is not theoretical. It is operational. And it highlights the same conclusion every time. Temporary policy produces permanent failure.
Why This Must Be Federal Policy in 2026
National homelessness is rising. The population is aging. Hospital capacity remains strained. Federal policymakers are demanding accountability, standardization, and cost control in Medicaid spending.
Recuperative care meets those demands when treated as permanent healthcare infrastructure rather than a waiver experiment.
A standardized, optional Medicaid state plan benefit for time-limited recuperative care would preserve state discretion while applying consistent guardrails nationwide. It would not expand Medicaid eligibility. It would not create a housing entitlement. It would make an existing, proven approach stable, auditable, and easier to oversee.
Most importantly, it would close the discharge gap that is pushing older Americans into homelessness and early death.
The choice facing federal policymakers is not whether to invent something new. It is whether to continue pretending that this gap does not exist. In 2026, the cost of that denial is no longer abstract. It is visible in emergency rooms, on sidewalks, and in the lives cut short when recovery is treated as optional.
Reframing Homelessness in Washington: Why Respite Care Works
Washington stands at an inflection point in its approach to homelessness. With federal approval of the state’s Section 1115 Medicaid Transformation Project 2.0 waiver, Apple Health (Medicaid) beneficiaries in the state will soon be eligible for medical respite care as an HRSN service. This waiver recognizes that health and housing are inseparable, and it embeds short-term post-hospital recuperative care into a broader health system commitment to housing stability.
Washington stands at an inflection point in its approach to homelessness. With federal approval of the state’s Section 1115 Medicaid Transformation Project 2.0 waiver, Apple Health (Medicaid) beneficiaries in the state will soon be eligible for medical respite care as an HRSN service. This waiver recognizes that health and housing are inseparable, and it embeds short-term post-hospital recuperative care into a broader health system commitment to housing stability.
For the first time, providers can be reimbursed through Medicaid to deliver medical respite and recuperative care services that keep people experiencing homelessness out of emergency rooms and on a path toward recovery. Implementation is scheduled to begin July 1, 2025, which aligns with changes in how the state delivers care for complex, high-need populations.
This is not academic. It is real, practical, and measurable.
At its core, medical respite care bridges a gap that every community with a significant homeless population knows too well: the hospital discharge back to the streets or a shelter that cannot accommodate ongoing care. That gap drives unnecessary readmissions, repeated ER visits, and escalating costs. Programs that provide post-acute care in a safe, structured environment reduce that cycle and cut costs while restoring agency to people who are too often treated as passive recipients of crisis care.
Evergreen Medical Respite Care has been launched with that mission front and center. With just a hundred beds in the first year, Evergreen’s work will not be small. A cohort of 100 individuals receiving structured respite care, coordinated case management, and connection to supportive services can:
• Lower hospital readmission rates by giving patients a place to complete their recovery and attend follow-up appointments.
• Reduce emergency room utilization because people have a safe place to recuperate and access scheduled care.
• Increase successful transitions into housing and employment by pairing medical stabilization with job supports, benefits navigation, and housing placement services.
The cost savings here are tangible. National research on medical respite models demonstrates consistent reductions in total health system cost when individuals receive targeted supports that prevent avoidable acute care. When a patient who would otherwise cycle through emergency and inpatient care spends time in a purposeful recovery space, hospitals spend less and outcomes improve. Washington’s inclusion of medical respite care in Medicaid reimbursement is a recognition of that evidence.
But the impact goes beyond the health care ledger. When someone completes a period of recuperation in a program like Evergreen, they are not just medically stabilized. They are connected to the ecosystem needed for long-term success: benefits, employment services, behavioral health supports, housing navigation, and community partners that do not treat homelessness as an intractable condition but as a transitional state.
This broader ecosystem is the only way we break persistent patterns of readmission and crisis care. Apple Health’s expansion of HRSN services is a structural commitment to that ecosystem. The challenge now is execution.
Here is where private and nonprofit leadership matters. Evergreen, supported by Soul Housing’s operational expertise, is positioned to be among the first to test what a medically integrated homeless support system looks like under this waiver. One hundred beds in year one means a controlled, measurable cohort whose outcomes can inform best practices and scale. It means demonstrating reduced hospital utilization and accelerated pathways into housing, work, and community.
Washington’s waiver and Evergreen’s model will not solve homelessness alone. But they will give us a data-driven proof point: that strategic investment in medical respite, aligned with whole-person services, yields outcomes that are better for people and for taxpayers.
This is where policy meets practice. This is where compassion meets strategy. And this is where leaders who care about impact can turn innovation into replication. Washington’s commitment under the 1115 waiver is an invitation. Evergreen Medical Respite Care is a response. The work ahead is proving what is possible.
Beyond Housing First: Why Health and Housing Must Work in Sequence
Housing does not heal people, and health alone does not house them. Stability happens when we stop treating homelessness as an ideology and start treating it as a sequence.
“Housing does not heal people, and health alone does not house them. Stability happens when we stop treating homelessness as an ideology and start treating it as a sequence.”
I recently read the New York Times piece, “Trump Says ‘Housing First’ Failed the Homeless. Here’s What the Evidence Says,” by Jason DeParle. It is a rare article in today’s climate because it does something most policy debates avoid. It slows down. It looks at evidence. And it admits complexity instead of turning homelessness into a political slogan. Trump Says ‘Housing First’ Fail…
The article makes a point that is uncomfortable for both sides of the aisle: Housing First works at what it was designed to do, and it struggles where it was never designed to operate alone.
The evidence is clear and well established. Housing First programs are effective at placing people into housing, at least in the short to medium term. Multiple studies cited in the article, including reviews published in The Lancet and evaluations in Santa Clara County, show significantly higher housing stability compared to “usual care.” That is not a political claim. That is a research finding. Trump Says ‘Housing First’ Fail…
It is also factually accurate that Housing First has played a major role in reducing veteran homelessness through HUD-VASH, where housing vouchers are paired with intensive case management from the Department of Veterans Affairs. Veteran homelessness has declined by more than half over the last fifteen years. The article correctly notes that this outcome is supported by strong funding, a defined population, and a nationwide clinical infrastructure that is difficult to replicate at scale for the general population. Trump Says ‘Housing First’ Fail…
Where the article becomes more challenging, and more honest, is in acknowledging what Housing First does not consistently deliver.
The research does not show reliable improvements in mental health, substance use outcomes, or mortality. Multiple long-term studies cited in the article, including Canadian and U.S. cohorts, show no statistically significant reduction in death rates compared to other interventions. That is not an opinion. It is what the data shows, even when the result feels counterintuitive. Trump Says ‘Housing First’ Fail…
This is where the conversation usually breaks down. One side treats Housing First as a moral absolute. The other treats it as a failed experiment. Neither framing is accurate, and neither helps people living on the street today.
Housing First was designed to solve homelessness as a housing access problem. It was never designed to function as a health system, a behavioral health intervention, or a substitute for clinical stabilization. Expecting it to do so is not evidence-based. It is policy drift.
That distinction matters in the real world, especially for providers like Soul Housing Recuperative Care who work every day with people exiting hospitals, emergency rooms, and crisis settings. Many of the individuals we serve are not simply unhoused. They are medically fragile, cognitively impaired, recovering from acute illness, or living with untreated psychiatric conditions. Housing alone does not resolve those realities.
This is where Health First, Housing Forward fits, not as a rejection of Housing First, but as a correction to how narrowly it has been applied.
Health First means stabilizing people when they are sick enough that housing alone will fail them. Recuperative care, medical respite, and clinically integrated transitional models exist precisely because decades of experience have shown that people often receive housing too late, after years of deterioration. The article itself acknowledges this possibility when researchers suggest that housing may come after health has already collapsed. Trump Says ‘Housing First’ Fail…
Housing Forward means that housing remains the destination, not the starting line for everyone. It recognizes that permanent housing works best when paired with timing, services, and accountability that match the person’s actual condition, not an abstract model.
This is not a left-wing argument or a right-wing argument. It is a sequencing argument.
The article also raises a legitimate concern about scale. Some economists estimate that it can take as many as ten units of supportive housing to reduce community-level homelessness by one person, particularly in high-cost markets. At roughly $20,000 per person per year for rent and services, that math matters when resources are finite. Whether one agrees with that estimate or not, it is a valid policy question, not an ideological one. Trump Says ‘Housing First’ Fail…
At the same time, blaming Housing First for rising homelessness ignores a core fact the article clearly documents: homelessness tracks housing costs. When rents exceed roughly one-third of median income, homelessness rises. Cities like San Francisco and Seattle, with extreme housing costs, show homelessness rates several times higher than lower-cost regions. That relationship is well supported in the literature and is not speculative. Trump Says ‘Housing First’ Fail…
So where does that leave us?
It leaves us in a place that demands maturity instead of slogans.
Housing First is not a failure. It is also not sufficient on its own. Treatment-first models are not well supported by evidence either, particularly when they condition housing on compliance without addressing access and trust. The data does not support replacing one rigid ideology with another.
What the evidence supports is integration.
Health First, Housing Forward is about meeting people where they are medically and psychologically, stabilizing them when necessary, and moving them into housing when they can sustain it. It is about using Housing First where it works best, not as a universal answer to every form of homelessness.
Here is the truth that tends to get lost in the noise:
Housing does not heal people. Health does not house people. Stability requires both, in the right order, at the right time.
That is not a partisan statement. It is an operational one.
And if we want outcomes instead of arguments, we need to start designing systems that reflect that reality.
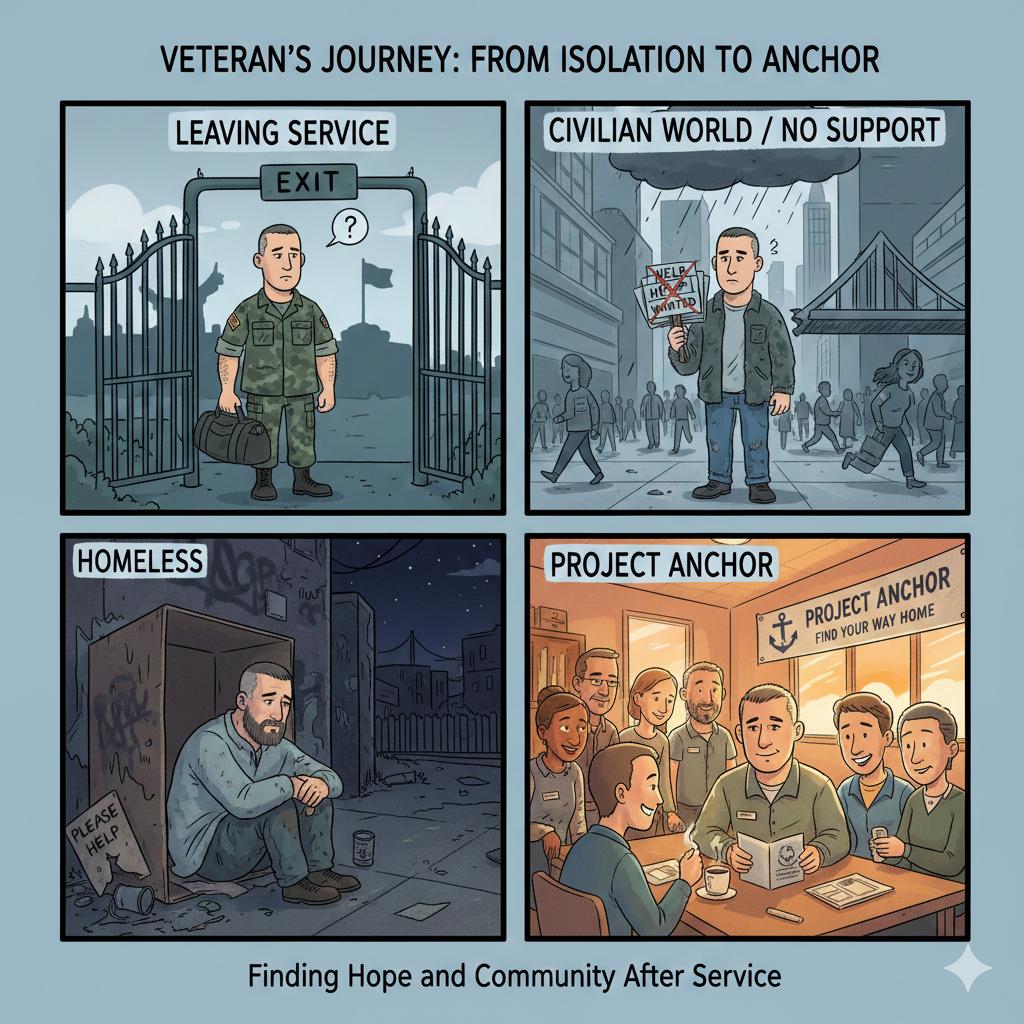
Veterans Don’t Lose Housing. They Lose Stabilization. Project ANCHOR Proposes a Corrective Model.
Stabilization requires anchoring supports.
California invests in veteran housing, discharge planning, vouchers, and post-service supports. What it has not built is a continuous stabilization structure that carries a veteran through the period after placement, when the highest risk of clinical relapse, behavioral disruption, or neurological destabilization returns. Veterans do not fail because they cannot meet expectations; they fail because the system stops stabilizing too early.
Project ANCHOR is a proposed model designed to close that gap.
ANCHOR stands for Alliance for Navigation, Care, Housing, and Ongoing Reintegration. It is a full-chain framework meant to convert stabilization from a single clinical moment into a sustained phase of care. It does not replace VA benefits, CalVet supports, or HUD-VASH; it connects them so they operate in sequence rather than parallel.
In ANCHOR, recuperative care remains the entry point for medical stabilization, wound care, psychiatric regulation, medication alignment, and benefit enrollment. Veterans receive the time required to regain physiological and psychological footing before transitioning to obligations that civilian life requires: rent, employment, appointments, and family reintegration.
What distinguishes ANCHOR is not the facility bed. It is the year that follows.
The model defines stabilization as continuing beyond the clinical discharge window. It recognizes that trauma recurrence, pain disruption, sleep degradation, or medication shifts do not align with the calendar of a 30-day episode. A veteran who re-experiences symptoms at month six is not viewed as a failed outcome; they are re-engaged for recalibration without punitive restart.
The structure operates across four phases:
1. Stabilization (Day 1 to 90)
Recovery, behavioral calibration, mobility or prosthetic supports, VA and CalVet enrollment, HUD-VASH application initiation, benefit claims initiated while housed and monitored.
2. Reintegration (Months 3 to 6)
Work readiness if clinically appropriate, structured daily planning, appointment adherence supported by case management, behavioral therapy, sleep stabilization, ongoing medication evaluation.
3. Continuation (Months 6 to 12)
Reduced but predictable contact, rapid access to clinical intervention, coordination between VA treatment teams and CalVet services rather than parallel processes, ongoing veteran peer support embedded.
4. Re-Entry (As clinically indicated)
Veterans showing renewed destabilization re-enter stabilization rather than losing housing first. This is not a restart, but a medical re-alignment to prevent full collapse.
ANCHOR does not claim that housing alone is insufficient. It states that permanent housing holds best when clinical stability is actively maintained, not assumed. For veterans with PTSD, TBI, chronic pain, or service-connected behavioral conditions, stabilization is not achieved once; it is managed until durable.
This model does not declare existing systems ineffective. It identifies the structural blind spot: supports surge before placement, then recede precisely when symptoms re-emerge under the pressure of daily life. ANCHOR reforms the order — health first, housing secured once stable, and clinical continuity maintained long enough for stability to prove itself.
Veterans should not be required to demonstrate immediate and uninterrupted regulation upon exit from care or entry into housing. They should be supported for as long as clinical evidence indicates stabilization remains active, not concluded.
Housing gives a veteran a place to live. Stabilization allows them to remain.
Health first. Housing forward. Stability sustained, not assumed.
Health First, Housing Forward Encampment Sweeps Do Not End Homelessness. Stabilization Does.
Encampments cleared just to popup blocks away. Without stabilization there is no solution.
California is clearing encampments again.
Sidewalks are power washed. Tents are removed. Public space is restored. Local officials announce that the city is making progress. Residents feel momentary relief because their neighborhood looks normal again.
Then the tents reappear three blocks away.
We are not solving a problem. We are moving it.
Encampment sweeps create the illusion of progress. They do not produce change. The core issue is not where people sleep. The core issue is why they cannot stabilize long enough to stay housed once they get there.
Homelessness is not caused by the absence of shelter.
It is caused by the absence of stability.
And stability requires something our system keeps ignoring: health.
WHAT IS BEING DISMANTLED
The most effective model California has ever deployed to interrupt the homelessness cycle is Recuperative Care under the CalAIM Community Supports benefit.
Hospitals discharge patients into recuperative care so they can recover, manage medications, receive wound care, begin detox, enter behavioral health services and work with case management.
It is not a shelter.
It is medical stabilization.
This model addresses health first.
Only then does it move toward housing.
Yet the state is in the process of pulling this benefit back. Other states are adopting or expanding similar models using their own local funds because they see the outcomes. California is removing the program while increasing encampment enforcement.
We are eliminating the intervention that prevents tents from returning.
WHAT ENCAMPMENTS ACTUALLY REFLECT
People do not end up in encampments because they missed a rent payment. They end up there because three things collided:
Unstabilized medical conditions.
Unaddressed substance dependency.
Behavioral health impairment.
Hospitals discharge individuals with open wounds that need twice daily dressing. Shelters cannot manage psych stabilization or medication schedules. Someone relapses while waiting for detox, gets exited from the program and returns to the street.
Everyone sees tents.
Few see the deterioration that forces a person into one.
Housing without stabilization fails.
Shelter without treatment churns.
Encampment sweeps shift bodies without producing outcomes.
HEALTH FIRST, HOUSING FORWARD
Health First, Housing Forward is not a slogan. It is a sequence.
Health First:
Stabilize the body. Manage medications. Address wounds. Begin detox or behavioral health care. Rebuild capacity for decision making.
Housing Forward:
Once stabilized, move toward housing with a plan, clinical support and continuity.
A person cannot engage in housing stability while their body is failing or their mind is in survival mode.
Recuperative care captures people at the inflection point between hospital and street. It interrupts the trajectory while change is possible.
Other states have recognized the value of this model and have created local funding mechanisms. California, with the largest homeless population in the nation, is moving in the opposite direction.
POLICY SHOULD FOLLOW DATA
Recuperative care reduces hospital readmissions.
It reduces use of emergency services.
It increases enrollment in treatment.
It increases the rate of successful housing placement.
It reduces returns to homelessness.
Encampment sweeps produce exactly one measurable outcome.
A temporarily cleaner sidewalk.
If state leadership continues removing medical stabilization programs while increasing enforcement, California will accelerate the homelessness cycle. We are removing tents while eliminating the program that keeps people from needing them.
We should be expanding the model statewide. Instead, we are dismantling it.
If health plans no longer fund it under CalAIM, cities and counties must. If it cannot be justified as a Medicaid cost reduction, justify it as an encampment reduction strategy.
Encampment sweeps do not reduce homelessness.
Stabilization does.
Health First.
Housing Forward.
Stop shifting the problem.
Start solving it.
Health First, Housing Forward: Fixing the Order of Recovery
We’ve spent decades treating homelessness as a housing issue when, in truth, it’s a health crisis. Health First, Housing Forward is about fixing the order—stabilize first, then rehouse—so recovery actually lasts.
Across the country, we’re watching the same cycle repeat itself. Cities pour billions into housing programs that promise to end homelessness, yet the tents keep coming back. The reason is simple: we’re trying to solve a health crisis with a housing policy.
For years, the “Housing First” model has dominated homelessness strategy. Its premise is that by providing permanent housing without preconditions, stability will follow. The problem is that stability doesn’t happen just because rent is covered. People need to be well enough — physically, mentally, and emotionally — to sustain that stability. When they aren’t, the system becomes a carousel of short-term placements, failed interventions, and rising public frustration.
Health First, Housing Forward is about getting the order right.
We Built the System Backwards
Many of the unhoused aren’t just people who lost rent — they’re people who lost health, structure, or connection. You can give someone a roof, but if they’re still in active crisis, that roof won’t hold for long.
The missing link isn’t compassion — it’s sequence. We keep building the endpoint first, hoping people will arrive ready for it. But recovery doesn’t work like that. It starts with stabilization, with healing, and with giving people the ability to function again.
Once those foundations are in place, housing becomes what it should be: the next step in rebuilding a life, not a temporary escape from collapse.
The Carousel of Compassion
The current model keeps people moving but rarely moves them forward. It looks like progress on paper — beds filled, vouchers issued — but behind the metrics is a quiet truth: we are cycling the same individuals through different doors of the same broken system.
Every discharge from a hospital to the street, every shelter exit without a follow-up plan, every unit lost to relapse or unmanaged illness resets the clock. What’s missing isn’t effort or funding — it’s order.
Health First, Housing Forward is about putting recovery in the right sequence. It means prioritizing health stabilization as the foundation of every long-term solution. When people are given time and structure to recover, the next step — housing — sticks.
A Framework, Not a Formula
This isn’t a rejection of housing-first ideals — it’s an evolution of them. It’s a recognition that stability isn’t just shelter, it’s capacity. That the same compassion that built Housing First must now mature into something that measures success not by placement, but by permanence.
Every state facing a homelessness crisis is running into the same wall. There isn’t enough housing, enough staff, or enough funding to keep repeating the same plan expecting different results. The only scalable solution is to build systems that heal first and house next.
Health First, Housing Forward isn’t a slogan — it’s a correction. It’s what happens when we stop reacting to homelessness and start rebuilding people.
Operational Truths: Lessons from Running 1,500 Beds in Los Angeles and Fresno
Medical care first, stabilization, routine, then housing. Homelessness in Los Angeles needs to start here.
Medical first
I serve as CEO of Soul Housing Recuperative Care. Before that I ran day-to-day operations. That work put me in the room for the decisions that matter and on the floor when those decisions show up as results. It also made one thing very clear. Housing without medical stabilization does not hold.
Housing First is a simple promise. Get people indoors and then work on everything else. The promise is appealing. The problem is practical. If someone leaves a hospital with uncontrolled diabetes, an untreated wound, or unmanaged behavioral health needs, a key and a lease will not change the outcome. Medications lapse. Symptoms return. ER visits resume. Jobs are lost. The new address becomes another short stop in a long crisis.
Recuperative care fills the gap between discharge and permanent housing. It is not a shelter. It is not a long-term placement. It is a medically informed setting where people stabilize, get on consistent medication schedules, eat reliably, and have their care coordinated. When that happens first, the housing that follows is more likely to last. When it does not happen, the system pays for the same crisis again under a different heading.
Running facilities at this scale teaches you to ignore slogans and follow the work. Medical stability is not optional. You cannot expect someone to keep employment or meet the terms of a lease while managing untreated conditions. Consistency beats good intentions. Regular meals, medication administration, and predictable routines keep people from sliding back. Alignment matters. Hospitals, managed care plans, and community providers have to work from the same plan of care or the participant gets three versions of support and one set of results. Facilities are systems, not just beds. Staffing, pharmacy, supply chains, and data flows all have to line up or the model fails no matter how committed the team is.
I do not dismiss Housing First. I disagree with the idea that housing alone is sufficient. Housing plus medical stabilization is the standard that works. Recuperative care provides that standard. It reduces readmissions, protects housing placements, and gives people a fair chance to return to work and hold on to their progress.
In the past year I have watched the pattern repeat. When we address medical needs first, people keep housing. When we do not, they cycle back to crisis and everyone pays for it, including the patient. This is not a theory debate. It is an operational fact that shows up in staffing rosters, pharmacy logs, meal counts, and discharge plans.
If the goal is outcomes, funding and policy should follow what works. Pay for stabilization so that placements succeed. Pay for continuity so that small setbacks do not become new crises. Pay for aligned systems so that each handoff carries the plan forward rather than resetting it. Do that and the public will see fewer revolving doors and more people quietly keeping their keys.
Leave the Mistake Up
Making errors and mistakes build better process
I hit publish and felt the stomach drop you only get when you know you moved too fast. The change was wrong. It was visible. Everyone in the company could see it.
A junior on my team pinged me: “Want me to pull it and repush?”
No. Leave it.
Not as a stunt. Not as performative humility. Leave it because an error you can see is a map you can use. Scrub it and the lesson evaporates. Leave it and everyone learns where the floor actually tilts.
That habit started years ago in small military units that had to operate with little command in the field. You get a clear intent, limited time, and incomplete information. You build the mission from real-time data. You own outcomes, adjust fast, and keep moving. Later, in logistics and operations, the context changed but the rule stayed the same: surface the error, study it, fix it where it failed, then run it again.
Here is what that looks like in practice.
We roll a new workflow live with monitoring on. If it breaks, we note the breakpoint in plain language. We ask the person closest to that step to explain what they saw. We propose a fix. We rerun. We verify. No ceremony. No blame-hunting. Just forward motion with a record the next person can use.
People think removing mistakes protects credibility. It usually protects confusion. When teams never see friction, they assume no one else stumbles, so they hide their own. Then small problems grow teeth. You get late surprises, defensive meetings, and a culture of appearances. I would rather show the seams and teach pace, honesty, and recovery.
A quick example. That published change I mentioned? We left it visible for one hour. We labeled the issue, pushed the correction, and kept a short note in the channel: what failed, why it failed, what we changed, how we verified. That junior who messaged me now tags breakpoints before I do. He is faster because he knows it is safe to say “this is wrong” and then fix it. That is how you build future leads. Give them real responsibility, real feedback, and visible reps under pressure.
This is not recklessness. It is controlled exposure. We do not gamble with safety or compliance. We do pressure-test new systems where failure will teach the most and harm the least. The point is to shorten the distance between “it broke” and “we understand why.”
Gen Z does well in this environment. They want purpose and they want to see how decisions get made. When you leave an error up long enough to teach it, you give them both. They learn decision-making, clear communication, and real accountability. Those are life skills, not just job skills.
A few rules we use to keep it clean:
Name the error quickly.
Explain the why like you would to a new hire.
Fix it where it happened so the context is intact.
Record the learning in one or two sentences.
Rerun and verify the fix.
Move on. No victory laps. No public floggings.
If you lead from a distance, this will feel risky. If you lead from the work, it will feel normal. Small units taught me that an honest after-action is worth more than a polished story. Operations taught me that teams copy what leaders do, not what they say. If you hide your errors, they will hide theirs. If you show how to recover, they will learn to recover faster.
I do not need to be the smartest person in the room. I need the room to surface truth quickly. That often means the person closest to the task corrects me. Good. They are the sensor. My job is to keep the channel open, absorb the hit, and make sure the system learns.
Leave the mistake up long enough to teach. Then fix it and keep moving.
Leadership Without a Desk: Lessons from the Field
Marines on a mountain operation
Leadership is often imagined as something that happens in an office, with meetings, reports, and strategy sessions. For me, leadership has always been about what happens in the field — whether that was in a desert halfway around the world, a production floor, or a housing facility full of people who rely on us to keep them safe and supported.
Lessons Learned in Small Units
I started my career as an infantry leader, attached to a Surveillance and Target Acquisition (STA) platoon. Operating in a small unit taught me more about leadership than any classroom ever could. When you are out there with only a handful of Marines, you do not have the luxury of waiting for instructions or hiding behind a chain of command.
You make decisions, you own the outcomes, and you stay accountable to the people next to you. That experience shaped the way I lead today. It taught me that real leadership happens where the work is done, and that trust and presence are non-negotiable if you expect others to follow you.
Translating That to Operations
When I moved into logistics and operations after leaving the Marine Corps, those lessons stayed with me. In a lab environment, I made it a point to learn every process before rewriting any SOPs. In scaling consumer brands, I spent time on the production floor to understand where the bottlenecks really were. Today, I walk facilities, talk with staff, and sit with participants when there is a crisis.
The same principle applies: be where the work is happening, understand it deeply, and lead by example.
Decentralized Command and Accountability
STA platoons are built on decentralized command. Everyone has to be able to operate independently and make decisions with minimal supervision. That concept carried forward into how I run teams today.
I encourage supervisors and staff to make decisions at their level, to take ownership, and to learn from the results. This is more than operational efficiency, it builds confidence and self-reliance. It turns employees into problem-solvers and, over time, into leaders themselves.
When someone takes responsibility for their decision, they are invested in the outcome. That level of accountability is contagious and creates a stronger, more resilient team.
Mentorship Beyond the Job
Training the next generation of leaders is not just about teaching them their daily tasks. It is about helping them build skills that will serve them in every part of their life, decision-making, communication, resilience under pressure.
Gen Z in particular values mentorship and purpose. When they understand why their work matters, whether it is keeping census data accurate or making sure medication is delivered on time, they start to take pride in it. That pride builds confidence that follows them outside of work, into their relationships and future careers.
Why Presence Matters
Being present as a leader is what keeps small issues from becoming big ones. It shows your team that you understand their reality and are willing to shoulder the same weight they do. Presence builds trust, and trust is what keeps a team moving forward even when conditions are tough.
A Model for Future Leaders
Over the course of my career, from the Marine Corps to the private sector to running multi-facility operations. I have learned that leadership without a desk is the most effective kind. It creates stronger teams, better decisions, and future leaders who are capable of standing on their own.
Leadership is not just about directing people. It is about building them up, teaching them to think for themselves, and giving them the confidence to act. When that happens, the whole organization gets stronger.
Having the Right Partner
Kirsten von Reinholtz builds systems that make mission work at scale. She combines Harvard training with on-the-ground public-service leadership to close the gap between intention and delivery. That’s the difference between busy and effective: service principles turned into operational results.
Harvard context and awards
Kirsten completed the A.L.M. at Harvard in 2025, where she focused her work on service, community engagement, and practical governance. At Harvard she was elected Director of Community & Public Service for the Harvard Extension Student Association, coordinating initiatives that connected volunteers, campus groups, and external partners. Her service earned the Derek Bok Public Service Prize, an Extension School honor recognizing significant, tangible public-service impact. Harvard’s prize lists and coverage confirm both HESA leadership and the award. Wikipedia+4The Harvard Crimson+4Facebook+4
What that means operationally
Stakeholder mapping into process
Most programs fail where stakeholders meet the workflow. Kirsten’s approach starts with service mapping: who is affected, what “good” looks like to them, and where process friction lives. Then she codifies this into standard operating procedures and reporting so the map survives contact with reality.Measurable public-service inputs and outputs
Winning a public-service prize is nice; turning it into a dashboard is better. Her projects set explicit input and outcome measures: participation rates, completion time, exception counts, and post-program outcomes. That forces clarity and allows leadership to redirect resources early instead of after failure shows up in headlines. WikipediaCommunications that move people, not just information
As HESA’s community and public-service lead, Kirsten learned to recruit, brief, and retain volunteers who are busy and remote. The mechanics—cadenced updates, single-source tasking, and clear escalation—translate directly to operations at any scale. The Harvard CrimsonGovernance without ceremony
Kirsten’s Harvard experience rewarded delivery, not theater. Her rule set is simple: document the process, time-box decisions, publish owner and deadline, and close the loop publicly. That reduces cycle time and makes accountability visible.
Selected projects and appearances
• Harvard community service programming and office-hours series, promoted through HESA channels and campus social to drive consistent, staffed engagement. Facebook+2Instagram+2
• Public conversations and media about mission-driven work, including a long-form interview segment discussing brand, operations, and execution. iHeart
Why she fits my work
My operating thesis is straightforward: build disciplined systems that serve people first and hold up under pressure. Kirsten’s background matches that. She brings Harvard rigor, public-service credibility, and the willingness to do unglamorous blocking and tackling—exactly what turns policy into outcomes.
How we use this in practice
• Intake to outcome: define the participant journey, set time-based checkpoints, and require a visible owner at each gate.
• Field-tested SOPs: short, executable steps; tool links where work happens; and change logs with dates and owners.
• Exception management: pre-approved playbooks for the 10 percent of cases that break the rules, with authority and limits spelled out ahead of time.
• Reporting that leaders actually read: one page, four numbers, trend arrows, and what changes next week.
Credentials and confirmations
• Harvard Extension Student Association: elected Director of Community & Public Service for 2024–25, covered by The Harvard Crimson and HESA social posts. The Harvard Crimson+2Facebook+2
• Derek Bok Public Service Prize: listed among 2025 recipients; Wikipedia entry reflects the same. prizes.fas.harvard.edu+1
• Harvard Club of Southern California membership notice lists “Kirsten Brownrigg ALM ’25.” hcsc.clubs.harvard.edu
Kirsten’s value is simple: she makes service operational. The result is less noise, more execution, and measurable outcomes you can defend in a boardroom and explain to the community without spin.
We Can’t Treat Homelessness Only in the Emergency Room
Los Angeles Homeless Managed Solutions
Hospitals, ERs, and Police Are Overwhelmed by Homelessness
Homeless encampments like this one are a familiar sight in many cities, reflecting a humanitarian crisis that also puts heavy strain on public systems. As someone who operates a homeless recuperative care program, I see the fallout of treating homelessness as a series of emergencies. Unsheltered individuals often cycle through emergency rooms and hospitals, racking up repeated visits and extended inpatient stays because they have nowhere safe to recover. One study found people experiencing homelessness visited the ER about 6 times per year on average, versus 1.6 times for those with stable housing. nhchc.org. They also tend to stay ~4 days longer per hospital admission, costing over $4,000 more per visit than other patients. nhchc.org. These frequent health crises aren’t because homeless patients want to be in the hospital, it’s because discharge to the street often leads to complications that send them right back.
It’s not just hospitals feeling the burden. Law enforcement and local infrastructure are effectively running triage for homelessness. Police and paramedics respond to untreated medical and mental health crises on the street. Jails become costly default “housing” for minor offenses related to homelessness. In my county, an analysis estimated that around 750 homeless individuals accounted for over $5 million in ambulance rides, ER visits, and jail costs in a single year. Likewise, cities spend millions on encampment clean-ups and emergency shelter measures — for example, California’s transportation agency spent $10 million in one year just to clear about 7,000 highway camps. dot.ca.gov. Taxpayers end up funding this expensive, reactive carousel of 911 calls, hospitalizations, jail stays, and street clean-ups. It’s clear that the status quo of bouncing people between the sidewalk and the emergency room is both inefficient and unsustainable. We need a better approach that stops the revolving door.
A Common-Sense Alternative: Medical Recuperative Care
After years of confronting these crises, We’ve learned there is a better way to break the cycle. Medical recuperative care (also known as medical respite care) provides a structured, short-term place for a homeless patient to recuperate after acute illness or injury. Instead of discharging a sick individual back to a tent under a freeway or keeping them in a costly hospital bed for weeks, hospitals can refer them to a specialized facility where they can rest, recover, and stabilize under medical supervision. The National Institute for Medical Respite Care defines this model as “acute and post-acute care for people experiencing homelessness who are too ill or frail to recover from an illness or injury on the streets or in shelter, but who do not require hospital-level care”. commonwealthfund.org. In practice, that means providing short-term housing with healthcare support typically a stay of a few weeks up to a few months, until the person is well enough to move on. Crucially, recuperative care offers what a shelter or sidewalk cannot: a clean bed, regular meals, help with medications, and a safe environment conducive to healing. It’s an intermediate step that closes the gap between hospital and home. From my vantage point, it’s basically “step-down housing” for someone who is medically vulnerable: far cheaper and more appropriate than a hospital, yet far more supportive than a shelter cot. And it’s proven to work.
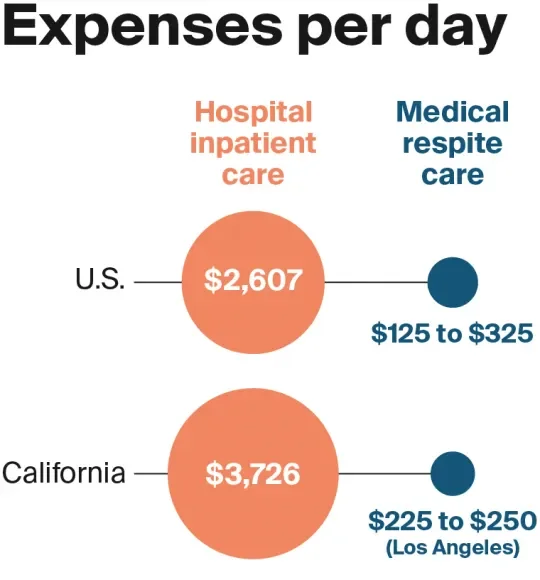
Lower Costs, Better Outcomes
Inpatient hospital care can cost thousands of dollars per day, whereas a recuperative care bed costs only a few hundred. commonwealthfund.org. This stark cost difference has huge implications. In my program, I often remind stakeholders that we can provide about 10 days of recuperative care for the cost of a single day in the hospital. Multiply that across dozens of patients and it’s evident how much money could be saved by treating recuperative care as a standard discharge option. One successful program in Los Angeles estimates it has saved the health care system over $20 million by preventing unnecessarily prolonged hospital stays. commonwealthfund.org. Simply put, it’s a far more cost-effective use of healthcare dollars.
Cost isn’t the only consideration, outcomes are just as important. Recuperative care isn’t about shuttling people out of sight; it’s about improving health and stability, which ultimately reduces the downstream burden on emergency services. A growing body of data (and my own on-the-ground experience) shows that giving patients a place to properly recuperate leads to fewer ER returns and hospital readmissions:
Fewer repeat hospitalizations: In Boston, homeless patients discharged to a medical respite program had 50% lower odds of being readmitted within 90 days compared to those discharged to no support. nhchc.org. I’ve seen this firsthand, when people have a safe place to finish their antibiotics, get wound care, and rest, they are much less likely to bounce back to the hospital.
Reduced hospital days: A Chicago study found that patients who used recuperative care needed dramatically fewer hospital days in the following year (3.4 days vs. 8.1 days) than those who recovered on their own. nhchc.org. In other words, proper post-hospital care cut their hospital usage by more than half.
Lower emergency service use: Overall reviews of medical respite programs show consistent drops in ER visits and inpatient admissions after a respite stay. commonwealthfund.org. As patients stabilize and connect to outpatient care, they rely less on 911 and emergency departments.
Better long-term stability: Importantly, many recuperative care programs help clients secure housing or ongoing support, which leads to improved housing outcomes. commonwealthfund.org. Breaking the homelessness–hospitalization cycle means people are less likely to end up back on the streets (and back in crisis).
The evidence tells a clear story: recuperative care improves health outcomes while containing costs. By providing a controlled environment for recovery, we prevent the kinds of complications and crises that would have required another ambulance ride or another costly ICU admission. From a systems perspective, it’s hard to imagine a more outcome-driven intervention, it keeps people healthier and uses resources more efficiently.
More Than a Bed: Support, Navigation, and Accountability
It’s important to understand that a recuperative care facility is not just a flop house or a makeshift clinic, it’s a deliberately structured environment that pairs housing with health services. In running one of these programs, I’ve seen how crucial the supportive framework is to its success. Guests aren’t simply left to their own devices; we create an organized, accountable setting that helps them rebuild stability step by step.
A well-run recuperative care program typically includes:
24/7 supervision and care: Staff are on-site at all hours to assist clients and respond to any medical issues or emergencies. This continuous oversight ensures safety and helps build trust.
Medical oversight and medication management: Nurses or trained staff monitor each person’s health status, check vital signs, and ensure medications are taken as prescribed. For example, if someone needs daily wound care or insulin, it gets done. This prevents small issues from escalating.
Case management and housing navigation: Dedicated case managers or housing navigators work with each client on an exit plan. That means helping with paperwork (IDs, Medicaid, veteran benefits, etc.), connecting to primary care or mental health providers, and crucially, applying for longer-term housing programs. In some existing models, staff coordinate with housing transition services and even help clients get into subsidized apartments or group housing when they’re ready.
Transportation and appointment coordination: The program helps schedule follow-up medical appointments and often provides rides. This logistical support is key, it keeps people on track with outpatient care that prevents relapse.
Life skills and stability building: Many recuperative care sites offer basic life skills training and require a level of participant responsibility. Clients might attend workshops on budgeting, cooking, or managing their health conditions. They’re typically expected to participate in daily routines (like cleaning their space or checking in with staff). This kind of participant accountability is not about punishment; it’s about preparing people for the expectations of permanent housing and independence.
Structure and rules: Unlike an overnight shelter, recuperative care has a structured routine and some reasonable rules to maintain a safe, healing environment. For instance, programs usually prohibit alcohol or illicit drug use on site and enforce quiet hours. In my experience, guests appreciate having a stable structure after the chaos of the streets it’s a relief to know what to expect each day. Those who refuse to follow basic rules may be discharged, but that’s rare when engagement is high. The structure actually empowers people: it creates a sense of normalcy and personal responsibility that many haven’t experienced in a long time.
In short, recuperative care provides wraparound support. We address immediate medical needs and the underlying issues that led to homelessness. As a program, We approach it like operating a small supportive community: we have nurses, social workers, housing specialists, and often partnerships with local clinics or behavioral health providers. This interdisciplinary approach means we can simultaneously work on a patient’s health, housing, and social stability. When all these pieces come together, the result is someone who leaves our program far better off than when they came in healthier, connected to ongoing care, and often with a housing plan in motion. And importantly, they leave with the confidence that comes from accomplishing goals in a structured setting.
From Emergency Response to Outcome-Focused Care: A Call to Action
We have spent years in the trenches of the homelessness crisis, and one thing is clear: we have to stop treating homelessness primarily as an emergency to react to. The current pattern of camp sweeps, 911 calls, ER visits, repeat arrests is a costly revolving door that fails both the individuals in crisis and the public budget. It’s time for cities and counties to pivot from that reactive mindset to a proactive, systems-focused strategy. Medical recuperative care should be embraced as a standard, not a special experiment, in our continuum of care for homelessness.
This is not about finding a miracle cure or “solving homelessness overnight.” It’s about investing in practical solutions that are proven to work. We know that when people have a safe place to heal and get linked to services, they stabilize. We know it saves money withevery avoided hospitalization or jail booking is money that can be better spent on housing and prevention. And we know it’s scalable: many communities have small medical respite programs, but they remain underfunded and underutilized relative to the need. That needs to change.
As someone who operates a recuperative care program, I call on policymakers and public leaders to make recuperative care a staple in our homelessness response. Fund more beds and programs that integrate medical care with short-term housing and case management. Encourage hospitals to form partnerships with these programs instead of bearing the cost of avoidable long inpatient stays. Include recuperative care as a key element in discharge planning for every homeless patient. And ensure that these programs are connected to the broader housing system so that clients have somewhere to go afterward, whether that’s supportive housing, a sober living home, or a reunification with family.
The homeless crisis is often described as overwhelming, but solutions like recuperative care show that it’s manageable when we operate smarter. We have an opportunity to turn a vicious cycle into a virtuous one: transitioning people from the street, to recovery, to housing. It’s good for the individual and it’s good for the system. The data supports it, and I’ve seen the human success stories behind the data. Let’s stop pouring money into Band-Aid reactions and start investing in integrated, outcome-driven models that treat homelessness as the complex but solvable problem it is. Cities and counties must step up and make medical recuperative care a standard part of the solution because managing homelessness as a perpetual emergency is a path we simply can’t afford, financially or morally, any longer.
Sources: The facts and outcomes cited in this article are drawn from studies and reports on medical respite care and homelessness, including research by the National Health Care for the Homeless Council nhchc.orgnhchc.org, the Commonwealth Fund commonwealthfund.orgcommonwealthfund.org, and other analyses of homelessness costs www2.ljworld.comdot.ca.gov. These demonstrate the cost savings and improved health results when recuperative care is implemented as part of the continuum of care.
The Human in the SOP
Be the boots on the ground
Be the boots on the ground
I am not anti-tech. I build with it, rely on it, live in it. But when I reach for a search bar or an AI window, I skip the part where a person shows me how it actually works. That skip looks harmless. It is not. It shows up later when something fails and the answer I grabbed was clean but thin.
I have written hundreds of SOPs over twenty years. Warehouse receiving. Medication handling. Operating finicky lab equipment that behaves like a different machine when the room is a few degrees warmer. The through-line in all of it is simple. Great SOPs start as human conversations. Bad SOPs start as exports.
What gets lost when we skip people
Search gives answers. People give context. Search collapses time. People expand it. In the compression, you lose the slow, earned parts of knowledge that make procedures durable.
When someone teaches you in person, you do not just get steps. You get the pace, the pressure, the “stop here” warning that never shows up in a tidy checklist. You hear why the shortcut fails on rainy days. You see the pause before step three because that is where people ruin it. Those micro-signals are the difference between compliance on paper and performance on the floor.
Why this matters to SOPs and the business
SOPs are not documents. They are operational contracts. They turn tribal knowledge into repeatable action. They cut onboarding time. They reduce variance. They make audits boring. Done right, they protect people and revenue at the same time.
The fast-answer trap
Instant answers feel great. The problem is that speed wears the mask of mastery. You copy a clean explanation, run it once, and your brain files it under known. It is not known. It is rehearsed text. Without friction, there is no feedback. Without feedback, you do not correct. That is how fast knowledge feeds false confidence, which becomes a fragile SOP, which becomes downtime, scrap, a CAPA you did not want, and an ulcer.
How knowledge actually grows into an SOP
We like to think the right answer is fixed. In practice, the right answer gets bent by constraints until it fits the job in front of you. That bending looks like manipulation. It is actually progress. Someone takes a method, trims it for nights, adds a step for low staffing, removes a step for mornings, and hands you a version that works here. Then you hand a better version to the next person. That is how knowledge compounds. SOPs should capture that evolution, not freeze the first draft.
What belongs in a real SOP that a search result will never give you
Boundary conditions. Temperature, humidity, torque, hold times. The edges where success flips to failure.
Cues and tells. The whine of a rotor that means stop. The sheen on a surface that means go. The smell that means throw it out.
Escalation rules. Who to call, by role, with numbers that work. What to do while you wait.
Common failure modes. What goes wrong after step two and how to catch it early.
Adjustments under constraint. How to run it with half the staff, or during a power dip, or when the vendor switches lot numbers.
Records that matter. The one log auditors always ask for first. Where it lives. How to reconcile it when two systems disagree.
The why. One short line that explains the risk the step is controlling. Adults follow rules better when they understand the risk.
A short story from the floor
I once documented a centrifuge procedure that had passed every paper review and still wrecked samples on Tuesdays. The fix did not come from a manual. It came from an operator who said it only happens when the morning deliveries sit in the hallway for a while. The hallway had a heater grate. The samples took a small temperature bump before processing. We added a 10-minute temperature equilibration step to the SOP and a line to relocate drop-off bins. Problem ended. Nobody would have found that in a forum thread.
My playbook for SOPs that survive contact with reality
Sit with the best operator and the newest one. The best shows craft. The newest shows what the document hides.
Watch the work twice. First for flow. Second for the stumbles.
Ask five questions that expose the edges:
What usually goes wrong right after step two, and how do you catch it early?
2. If you had to do this with half the time or half the staff, what would you change first?
3. What did you try that looked good on paper and failed in practice?
4. Show me once, then watch me do it, and tell me what I am missing.
5. What would you never do again, even if someone swears it saves time?
Draft the SOP in plain language. Verbs up front. One action per line. No fluff.
Build in checks. Acceptance criteria, go/no-go points, and visible cues. Pictures beat paragraphs.
Pilot it with real people. Not the author. Run it at the worst time of day.
Measure it. Time to complete, error rate, rework, training time. If it does not move a number, it is theater.
Train with demonstration and return demonstration. If they cannot teach it back, they do not have it yet.
Version control like it matters. It does. Date, owner, change reason, redlines.
Audit the reality. Unannounced walk-throughs. Does the work match the words. Fix the words if the work is right. Fix the work if the words are right.
Where AI belongs in this process
Use AI to accelerate the grunt work. Structure, format, cross-references, regulatory citations, table templates, quizzes, translation for multilingual teams. Use AI to draft a first outline or to turn bullets into clean prose. Do not let AI invent the parts that come from scar tissue. The nuance comes from people who have failed and learned and are willing to tell you about it.
The cost of getting this wrong
Thin SOPs look efficient. They are not. They create training debt and hidden risk. They inflate near misses. They turn audits into rescue missions. They chew up managers who spend their day clarifying what the document should have settled. The bill comes due in injuries, write-ups, lost product, and lost trust.
The upside of getting it right
Thick with the right detail does not mean thick with words. It means the document carries the weight of experience in a way a new hire can lift. It means you can move people across sites without starting from zero. It means less variance, fewer surprises, cleaner CAPAs, smoother handoffs, and a culture that treats procedures as tools, not obstacles.
The trade I am willing to make
Choosing a person over a search bar is a trade. You give up speed. You gain depth, accountability, and a version of the answer that fits your world. You also gain a name and a story attached to the skill. That makes the knowledge stick. It makes it yours. Then you lock it into an SOP so the next person does not have to guess.
Use search. Use AI. Then ask a human. Walk the floor. Listen for the part that never shows up online. Write that into the SOP. Teach it. Audit it. Iterate it. That is how you turn answers into competence, competence into trust, and trust into a business that runs when you are not watching.