America is at an inflection point in homeless healthcare
Over the past decade, homelessness policy has increasingly centered on housing as the primary solution. Housing remains essential and should always be the long-term goal. But as homelessness becomes more medically complex, behaviorally acute, and systemically entrenched, it is becoming clear that housing alone cannot carry the full weight of the response.
What is emerging now is not a left-right debate, but a systems problem.
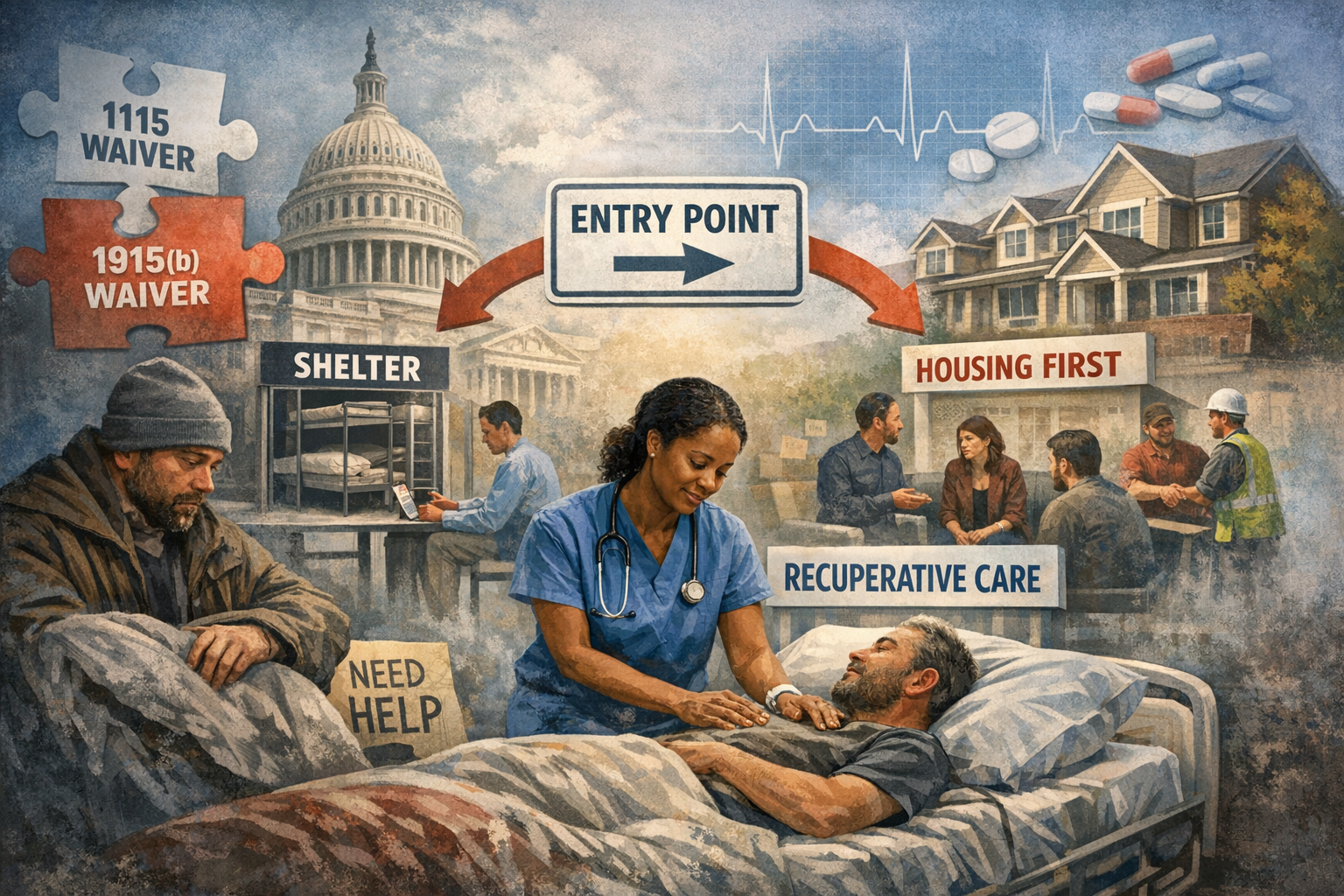
Across the country, communities are relying heavily on federal Medicaid waiver authority, particularly Section 1115 demonstration waivers and Section 1915(b) managed care waivers, to fund healthcare services tied to homelessness. These waivers have enabled critical innovations, including recuperative care, medical respite, enhanced care management, and housing-related supports. At the same time, they introduce uncertainty into a moment that demands stability.
Waivers, by design, are temporary. They are subject to renewal cycles, shifting federal guidance, state interpretation, and political change. Programs built on waiver authority often operate on short planning horizons, even as the populations they serve require long-term, consistent intervention. This mismatch is increasingly visible on the ground.
Healthcare providers, counties, and managed care plans are being asked to scale programs for people with complex medical, mental health, and substance use needs while funding structures remain provisional. The result is fragmentation. Services expand, retract, rebrand, and reconfigure, often faster than frontline systems can absorb.
This instability shows up most clearly at the point of entry.
In many counties, the Coordinated Entry System, or CES, functions primarily as a housing prioritization tool. It was designed to allocate scarce housing resources fairly, not to serve as a clinical or stabilization gate. Over time, however, CES has become the de facto front door for people with needs that extend well beyond housing.
This creates a structural gap.
Housing is the destination, but stabilization is the prerequisite. Many individuals experiencing homelessness are not immediately housing-ready, even when units are available. Untreated medical conditions, unmanaged mental illness, active substance use, and lack of basic daily functioning can make rapid placement unsuccessful or unsustainable. When stabilization is skipped, housing placements fail, costs rise, and individuals cycle back into crisis.
This is not an argument against housing-first principles. It is an argument for sequencing.
Stabilization does not mean delay or denial. It means meeting people where they are clinically and functionally, addressing acute needs first, and creating a realistic pathway to housing that can endure. Medical respite and recuperative care programs are designed precisely for this role, providing a short-term, structured environment where individuals can recover, stabilize, and reconnect to care before moving forward.
At organizations like Soul Housing Recuperative Care, this model is applied daily. Participants are referred not because they need housing, but because they need time and support to recover from illness or injury in a safe setting. During that window, medical care is coordinated, behavioral health needs are identified, substance use treatment options are engaged when appropriate, and basic routines are reestablished. Housing planning happens in parallel, not in isolation.
This approach highlights a broader lesson. Homelessness is not a single condition. It is the outcome of overlapping systems failures, including healthcare access, behavioral health capacity, workforce participation, and social support. Treating it as a housing logistics problem alone oversimplifies reality and limits outcomes.
The current reliance on 1115 and 1915(b) waivers reflects innovation, but also fragility. When core stabilization services depend on temporary authority, the entire continuum becomes vulnerable to disruption. Providers hesitate to invest, counties struggle to plan, and individuals experience inconsistent access to care.
What is needed now is not ideological realignment, but structural clarity.
Stable programs require stable authorization. Clear clinical gates must complement housing prioritization. Healthcare, behavioral health, and recovery services must be treated as foundational infrastructure, not auxiliary supports. And data must be used to evaluate not just placement speed, but durability of outcomes.
The next phase of homeless healthcare will be defined by whether systems can move from pilots to permanence. Housing will remain the goal. But without deliberate investment in stabilization, the system will continue to recycle people through crisis rather than resolve it.
This is the inflection point. The decisions made now about structure, sequencing, and permanence will shape outcomes for years to come.