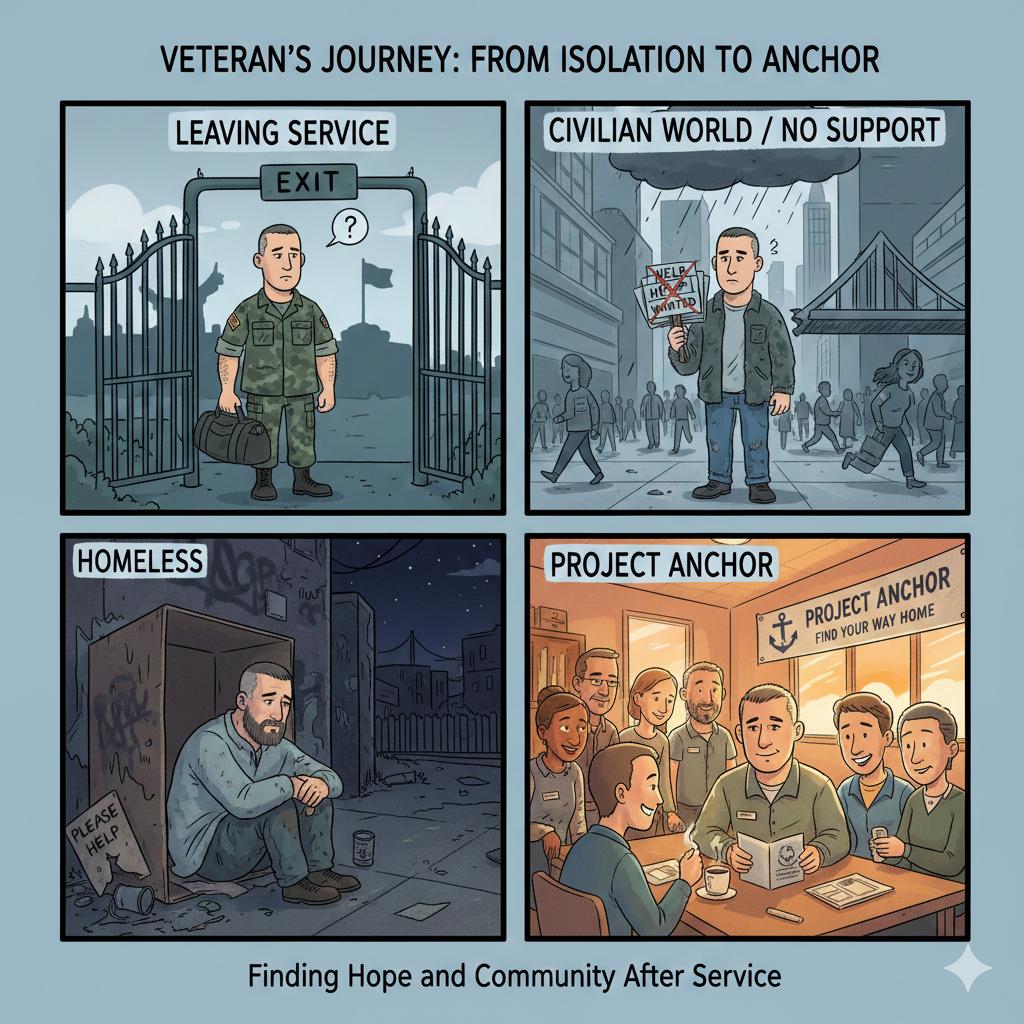
Veterans Don’t Lose Housing. They Lose Stabilization. Project ANCHOR Proposes a Corrective Model.
California invests in veteran housing, discharge planning, vouchers, and post-service supports. What it has not built is a continuous stabilization structure that carries a veteran through the period after placement, when the highest risk of clinical relapse, behavioral disruption, or neurological destabilization returns. Veterans do not fail because they cannot meet expectations; they fail because the system stops stabilizing too early.
Project ANCHOR is a proposed model designed to close that gap.
ANCHOR stands for Alliance for Navigation, Care, Housing, and Ongoing Reintegration. It is a full-chain framework meant to convert stabilization from a single clinical moment into a sustained phase of care. It does not replace VA benefits, CalVet supports, or HUD-VASH; it connects them so they operate in sequence rather than parallel.
In ANCHOR, recuperative care remains the entry point for medical stabilization, wound care, psychiatric regulation, medication alignment, and benefit enrollment. Veterans receive the time required to regain physiological and psychological footing before transitioning to obligations that civilian life requires: rent, employment, appointments, and family reintegration.
What distinguishes ANCHOR is not the facility bed. It is the year that follows.
The model defines stabilization as continuing beyond the clinical discharge window. It recognizes that trauma recurrence, pain disruption, sleep degradation, or medication shifts do not align with the calendar of a 30-day episode. A veteran who re-experiences symptoms at month six is not viewed as a failed outcome; they are re-engaged for recalibration without punitive restart.
The structure operates across four phases:
1. Stabilization (Day 1 to 90)
Recovery, behavioral calibration, mobility or prosthetic supports, VA and CalVet enrollment, HUD-VASH application initiation, benefit claims initiated while housed and monitored.
2. Reintegration (Months 3 to 6)
Work readiness if clinically appropriate, structured daily planning, appointment adherence supported by case management, behavioral therapy, sleep stabilization, ongoing medication evaluation.
3. Continuation (Months 6 to 12)
Reduced but predictable contact, rapid access to clinical intervention, coordination between VA treatment teams and CalVet services rather than parallel processes, ongoing veteran peer support embedded.
4. Re-Entry (As clinically indicated)
Veterans showing renewed destabilization re-enter stabilization rather than losing housing first. This is not a restart, but a medical re-alignment to prevent full collapse.
ANCHOR does not claim that housing alone is insufficient. It states that permanent housing holds best when clinical stability is actively maintained, not assumed. For veterans with PTSD, TBI, chronic pain, or service-connected behavioral conditions, stabilization is not achieved once; it is managed until durable.
This model does not declare existing systems ineffective. It identifies the structural blind spot: supports surge before placement, then recede precisely when symptoms re-emerge under the pressure of daily life. ANCHOR reforms the order — health first, housing secured once stable, and clinical continuity maintained long enough for stability to prove itself.
Veterans should not be required to demonstrate immediate and uninterrupted regulation upon exit from care or entry into housing. They should be supported for as long as clinical evidence indicates stabilization remains active, not concluded.
Housing gives a veteran a place to live. Stabilization allows them to remain.
Health first. Housing forward. Stability sustained, not assumed.